ISHAS Memorials
Overview
ISHAS wishes to recognize some of our past members who have significantly impacted the field of Hyaluronan Sciences.
Please click the names listed below in alphabetical order to view more information.
Endre Alexander Balazs, M.D., scientist, innovator, and entrepreneur, whose 70 years of pioneering research on the structure and biological activity of hyaluronan (hyaluronic acid) led to discoveries on extracting and purifying the molecule itself so that it could be used therapeutically, died Saturday, August 29, 2015 in St. Tropez, France. He was 95 years old.
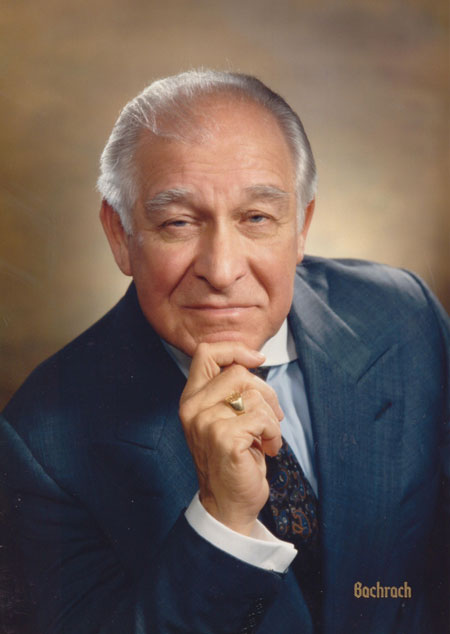 As the world’s leading expert on this important macromolecule, a viscoelastic glycosaminoglycan present in all tissues of the human body, it was his vision of how it could be used and his specific contributions that led to medical products that have benefitted millions of patients worldwide. In the 1970s he patented the “Non-Inflammatory Fraction of Hyaluronan” to be used therapeutically. The first of the therapeutic products, Healon®, made intraocular surgeries for cataracts and subsequent intraocular lens replacement almost routine, and was also the first viscosupplementation product for the alleviation of pain and improvement of mobility in arthritis. To this day Healon and other products he developed, such as Synvisc® for viscosupplementation in osteoarthritis, remain the most utilized products in their fields. Worldwide, these products have facilitated eye surgeries in more than 250 million patients, and more than 50 million patients crippled by osteoarthritis of the knee are now able to walk and live more comfortably and productively.
As the world’s leading expert on this important macromolecule, a viscoelastic glycosaminoglycan present in all tissues of the human body, it was his vision of how it could be used and his specific contributions that led to medical products that have benefitted millions of patients worldwide. In the 1970s he patented the “Non-Inflammatory Fraction of Hyaluronan” to be used therapeutically. The first of the therapeutic products, Healon®, made intraocular surgeries for cataracts and subsequent intraocular lens replacement almost routine, and was also the first viscosupplementation product for the alleviation of pain and improvement of mobility in arthritis. To this day Healon and other products he developed, such as Synvisc® for viscosupplementation in osteoarthritis, remain the most utilized products in their fields. Worldwide, these products have facilitated eye surgeries in more than 250 million patients, and more than 50 million patients crippled by osteoarthritis of the knee are now able to walk and live more comfortably and productively.
Dr. Balazs, born in Budapest, Hungary, received his medical degree from the University of Budapest in 1942. He launched his research career at the Department of Histology and Embryology of the University. In 1947 he continued his research at the Department of Experimental Histology of the Karolinska Institute in Stockholm. In 1951, at the invitation of Harvard Medical School, he moved to Boston to organize the Retina Foundation and set up research laboratories there, and later became its President. He was co-founder of the Boston Biomedical Research Institute where he worked from 1968-1975. Dr. Balazs moved to New York and continued his research and teaching at Columbia Presbyterian Medical Center as the Malcolm P. Aldrich Research Professor and Director of Research in the Department of Ophthalmology at the Harkness Eye Institute. Upon his retirement in 1987, he became the Malcolm P. Aldrich Research Professor Emeritus.
In 1968, Dr. Balazs founded Biotrics, Inc., to develop methods to produce and apply hyaluronan for medical purposes. In 1981, he co-founded Biomatrix, Inc. with his wife, Dr. Janet L. Denlinger. As the company’s Chief Executive Officer and Chief Science Officer, Dr. Balazs established a strong research and development program that focused on modifying hyaluronan, work that led to important therapeutic applications, including a new viscosupplement for arthritic joints (Synvisc®); Hylaform® and the concept of viscoaugmentation of dermal tissue for the treatment of facial wrinkles and depressed scars; and Hylashield® to be used on the surface of the eye to alleviate pain and irritation. After a public offering of stock in 1991, Biomatrix was listed on the Nasdaq stock exchange. Its subsequent financial success allowed Biomatrix to be listed on the New York Stock Exchange in July of 1998. In 1999 Biomatrix was recognized by Fortune magazine as one of America’s 100 Fastest- Growing companies. After Biomatrix was sold to Genzyme Corp. in 2000, Dr. Balazs continued his research and development work on hyaluronan at the Matrix Biology Institute that he and Dr. Denlinger founded as a charitable medical research institute.
At his initiative in 1962 the first international eye research journal, Experimental Eye Research, was founded with him serving as Editor-in-Chief until 1991. He also initiated and co-founded the International Society for Eye Research (ISER; 1974) and was its General Secretary and later its President. In 1986, the International Society for Eye Research established the Endre A. Balazs Prize and named him Honorary President of the Society. More recently (2004), he founded the International Society for Hyaluronan Sciences (ISHAS).
Dr. Balazs received many honors for his research/development and business accomplishments. He was a recipient of the Friedenwald Award from the Association for Research in Ophthalmology (1963); Guggenheim Fellow (1968) and Macy Foundation Scholar in 1991; the Cornelius D. Binkhorst Medal from The American Academy of Ophthalmology (1986); recognized by the American Arthritis Foundation as Humanitarian of the Year (1998); Herman F. Mark Technology Medal from the Polymer Research Institute of Polytechnic University, Brooklyn, NY (2003); Ellis Island Medal of Honor, NY (2004); In 2005 he was awarded the George Washington Award of the American Hungarian Foundation, which honors persons whose eminent contributions are in the broad field of human knowledge, the arts, commerce, industry, the sciences, and understanding men among men and nations; Distinguished Alumni Award from the Schepens Eye Research Institute (2008); induction into the Ophthalmology Hall of Fame by the American Society of Cataract and Refractive Surgery (2009); He became an external member of the Hungarian Academy of Sciences in the Section of Chemistry in 2010; received the Helen Keller Prize for Vision Research (2011); and in 2012, the New Jersey Inventors Hall of Fame recognized him for “Lifetime patent and technology achievement related to eye and orthopedic research and groundbreaking discoveries in utilizing hyaluronan for therapeutic purposes”. Just this year he was honored with a named chair, The Endre A. Balazs Professorship in Innovation and Entrepreneurship, at the Karolinska Institutet in Stockholm, Sweden. He was also awarded several honorary degrees: 1967: in Medicine, from the University of Uppsala, Uppsala, Sweden; 1991: in Medicine, from Semmelweis University for Science and Medicine, Budapest, Hungary; 2005: in Science, from Purdue University, West Lafayette, Indiana; 2009: of Humane Letters, from Saint Leo University, Saint Leo, Florida.
Author of over 300 publications in the fields of biochemistry, physicochemistry, rheology, pharmacology, biology and pathology and on the subjects of hyaluronan and sulfated glycosaminoglycans, radiation chemistry of carbohydrates, joint tissues and synovial fluid, eye tissues, especially the vitreous and cornea, and the medical applications of hyaluronan and hylans. He has received nineteen US and corresponding International patents in these fields.
He is survived by his wife, Janet L. Denlinger of Fort Lee, NJ and St. Tropez, France; his former wife, Eva K. Balazs; two children: Marianne E. Balazs and André T. Balazs; and four grandchildren: Johann W.E. Scheidt and Anna- Elisabeth E. Scheidt, Alessandra Ford Balazs and Isabel Ford Balazs.
Donations in Dr. Balazs’ memory may be made to the Endre A. Balazs Foundation. This will help to continue his legacy of support for scientific innovation and therapeutic applications of hyaluronan products for the benefit of all mankind.
Endre A. Balazs Foundation
c/o 9 Shore Road
Edgewater, NJ 07020
201-886-1562
We mourn the loss of ISHAS member, Mark Lauer, PhD
It is with great sadness that we report the death of our Cleveland Clinic colleague, Dr. Mark Lauer, in a tragic car accident on October 12, 2015. He was 42 years old. Mark is survived by his wife and five young children and leaves behind numerous colleagues and friends who recognized his promise and developed great respect for his achievements. Additionally, Mark was very well known for his great caring and kindness in the Lerner Research Institute as well as in his community, where he served as a deacon for his church.
Mark’s research career encompassed the fields of cell and matrix biology, and began, when he joined the laboratory of Dr. Kevin J. McCarthy at Louisiana State University as a graduate student, after earning his BA in Chemistry at Northern Kentucky University in 1997. Following completion of his PhD, Mark joined the Cleveland Clinic to continue with postdoctoral training in the laboratories of Aimin Wang (2001) and Vincent Hascall (2003), investigating the biology and pathology of extracellular matrix, focusing on heparan sulfate and especially hyaluronan.
Through his diligence and hard work, Mark rose steadily through the ranks at the Cleveland Clinic, to Research Associate (2009), Project Staff (2012), and Staff Scientist (2014) and was most recently promoted to Assistant Staff in the Pediatric Institute in June of this year. He collaborated with BME colleagues and with lung disease researchers studying, among other things, the immune system’s response to respiratory syncytial virus, a major source of infection in pediatric patients.
Mark was Principal Investigator of an R01 grant from the National Institute of Health to investigate TSG-6, a hyaluronan-binding molecule involved in inflammation. His work focused on inflammation and lung disease, especially cystic fibrosis. In addition, Mark was a co-investigator and core leader on a major Program Project Grant, one of only six nationwide under the NIH’s “Programs of Excellence (PEG) in Glycosciences. He coauthored more than 20 articles and held two patents on a promising method to treat airway inflammation.
ISHAS Community
Professor Glyn O. Phillips (1927-2020)
 Professor Glyn O. Phillips was born and brought up in Rhosllannerchrugog near Wrexham in North Wales, UK. Glyn was the son of a coal miner who became a Professor of Chemistry, being distinguished both as a scientist and as a leading figure at Higher Education Institutions around the world. He was the author of over 600 academic papers as well as author/editor of 43 books.
Professor Glyn O. Phillips was born and brought up in Rhosllannerchrugog near Wrexham in North Wales, UK. Glyn was the son of a coal miner who became a Professor of Chemistry, being distinguished both as a scientist and as a leading figure at Higher Education Institutions around the world. He was the author of over 600 academic papers as well as author/editor of 43 books.
Glyn graduated from Bangor University with a first-class honours degree in chemistry, where he also received a PhD and DSc for his research into carbohydrates. He was appointed as a lecturer in chemistry at University College Cardiff in 1954 and became Professor of Chemistry at the University of Salford in 1967. In 1970 he went to Nigeria to establish the University of Benin and was its first Vice Chancellor. He subsequently also set up research centres in both North Wales and China.
Glyn’s academic focus was on hydrocolloids, particularly on food hydrocolloids and medically related biopolymers of connective tissue, including hyaluronan. He was a long-standing collaborator and friend of Endre Balazs, and was involved in the production of HYLAN, an FDA approved product that was used for the replacement of synovial fluid damaged by osteoarthritis. Glyn was one of the founding members of ISHAS and the organiser of an International HA meeting in Wrexham in 2000. Following in his footsteps, his son, Aled Phillips, initiated research into hyaluronan in kidney disease at the University of Cardiff.
More about Glyn’s life can be found in the following links: https://www.wcia.org.uk/wcia-news/tribute-glynophillips/ and https://www.learnedsociety.wales/fellow/glyn-o-phillips/
 Professor Robert Stern MD- a long life of inspiring scientists to sift through the goo for what was clinically relevant.
Professor Robert Stern MD- a long life of inspiring scientists to sift through the goo for what was clinically relevant.
Many will mourn the loss of Robert Stern, but with the number of scientists and medical students he inspired over the years I am confident his memory still has quite a long healthy life ahead of it.
While Robert was a board-certified pathologist by trade and taught pathology to the medical students, many clinician scientists and doctoral candidates found their way to glycosaminoglycan biology through his laboratory in Health Sciences West at UC San Francisco over the years. In the early 1990’s, Robert’s laboratory in the Department of Pathology had assembled a mosaic of small grants along with some RO1s. The lab was well seasoned with chromatography columns of all shapes and sizes, buffer carboys, cold rooms and other basic biochemistry equipment from decades of experimentation, along with a tissue culture room that housed a museum quality coulter counter from the 1960’s. While perhaps not as modern as the neighboring cell, molecular and immunology labs in the department it was a remarkable scientific sandbox that Robert created for scientists setting out on their journey to solve medical challenges that might have a relationship to glycosaminoglycan biology.
Roberts lab meetings, (called ‘therapy sessions’ as I recall) were held in a small adjacent office that housed all the scientists together and was decorated with pathology artifacts, microscopes, countless racks of slides and parrafin blocks of rare pathologies. The -80C freezers were always overflowing with serum samples collected from fascinating diseases, many waiting for just the right hypothesis and analytical test to be thawed and tested.

Nearly every lab meeting was preceded with a lecture about a particular clinical observation on the hospital wards over the years. And every disease in Robert’s lab was observed through the eyes of the extracellular matrix. Some were anecdotal observations from publications back in the 1950’s and 1960’s, or the ‘golden age of carbohydrate chemistry’ as Robert defined it. But these clinical challenges and observations from the wards and old papers were rapidly devoured by eager young students that he inspired to start building hypotheses towards what might be a worthy experimental investigation.
Analytical tools were all applied in a similar way. First the clinical problem, then the blood or tissue samples arrived, then testing, followed by analysis of whether any association existed. With the analytical data in hand, new hypothesis developed. Was the abnormal laboratory value in a patient population a result of a stimulatory protein, an enzyme or an inhibitor? From there the long journeys often began.
A biochemical observation such as elevated tissue levels of hyaluronan during fetal development that might relate to scar-free wound healing, or how HA accumulation during ductal branching morphogenesis might link to cancer invasion were common early themes. Every clinical problem was viewed through the gooey lens of how the extracellular matrix or hyaluronan might be a culprit. In some cases, hypotheses evolved after retrospective analysis of clinical outcomes in malignancies to HA, hyaluronidase or CD44 splice variants. Some had diagnostic implications to treating patients more accurately. And others called for someone to go isolate the factor responsible.
There was a constant mantra from Robert when it came to solving biochemical problems. “Without a good assay there is nothing you can do, but with a great assay there is nothing you cannot do!”
Some of these assays had unique reagents that required everyone to participate in annual rituals, such as regenerating the annual supply of biotinylated hyaluronan binding protein or bHABP as it was known at the time. Bovine nasal cartilage would arrive, scalpels and dishes would be distributed, and all would join in to trim kilograms of nasal cartilage of contaminating tissue and prepare it for dissolution into potent chaotropic salts and trypsin with affinity isolation on HA resins. One wrong step and everything would have to start over. Worse yet, a subpotent batch might be generated that would be unsuitable for all of its great uses after calibration with the prior standard.
This biotinylated tryptic fragment of aggrecan in Robert’s lab was an analytical workhorse in the early days for every assay it seemed: histochemistry, measuring HA in samples and measuring hyaluronidase activity. In short, all the precious assays relied upon this fickle little reagent from a cows nose.
And in the ‘grind and find’ world of pathology, Robert’s lab required that all factors be isolated to homogeneity and characterized fully with careful accounting for loss or gains (removal of inhibitors) at each step along the way. Whether fractionating liters of conditioned cell media, extracting kilograms of porcine livers, spleens or lymph nodes, or even tens of liters of human plasma or hundreds of liters or urine in the cold room, the biochemical journey to purify the factor responsible was often a multi-year journey.
And when something came out that looked really pure and antibodies made then the gene had to be cloned the old fashioned way from peptide fragments and degenerate PCR. There were many projects that purified things some of the way but fell short of completion. The HA stimulating activity or HASA, which seemed to fall apart on columns faster than the bioassay could measure its potency in column fractions. Or the porcine liver enzyme that looked like it was a hyaluronidase but also looked remarkably very close to the hemopexin it really was. Nevertheless, the small laboratory was able to tease out entire hyaluronidase gene families after many years of grinding up tissues and made a number of remarkable contributions to the HA community. Roberts laboratory also made some truly remarkable findings surrounding HA associations in wound healing, cancer and fetal development that continue to fuel hypotheses to this today. Several medicines that are approved around the world can trace their roots back to Robert’s laboratory and many good scientists and clinicians emerged from his laboratory with so much enthusiasm about applying science to understand those clinical observations.
On the lighter side, it is also quite worth noting that Robert Stern was a truly exceptional writer. And he demonstrated exceptional pleasure when applying his red pen to any first draft a student hoped would be their finest work. I am confident this tribute will break nearly every rule he tried to instill into our scientific writing. But at a certain point, we must accept our limitations with the time we have available to correct or improve them. So the materials and methods are not perfectly organized, the conclusion loquacious, and the title quite boring indeed. But I think the content is still worthy of peer review.
Robert Stern provided guidance to many many people in the hyaluronan community. And he will be remembered by more than just his publications in the field.
